Not every patient who presents with an acute coronary syndrome (ACS) has obstructive atherosclerotic coronary artery disease. SCAD is frequently missed as a possible diagnosis, especially in younger female patients. Here are seven key points to remember on SCAD:
- SCAD is thought to be caused by either an intimal tear, which allows blood to enter and generate a false lumen, or a spontaneous haemorrhage arising from the vasa vasorum within the vessel wall.
- Chest pain and elevated cardiac enzymes along with ischemic changes are characteristic of the presenting ACS.
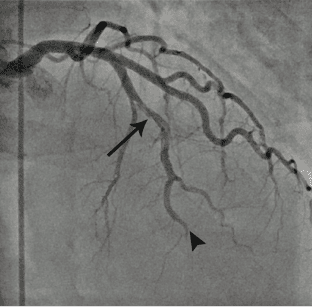
- Coronary angiography is recommended as a first-line diagnostic imaging method for early invasive management of ACS. Intravascular ultrasound (IVUS) and optical coherence tomography (OCT) can aid the diagnosis, but carry the risk of iatrogenic extension of the dissection.
- Conservative management should be considered in clinically stable patients without high-risk anatomy.
- Percutaneous coronary intervention (PCI) for treatment of SCAD is associated with an increased risk of complications and technical failure.
- In patients managed medically, most experts recommend aspirin for at least a year. Statin therapy is not recommended routinely after SCAD.
- Extra coronary imaging from the brain to the pelvis that includes extracranial carotid arteries and renal arteries is important given the high co-prevalence with fibromuscular dysplasia.