Transcatheter aortic valve implant/replacement
If you have been diagnosed with a condition called aortic stenosis, the aortic valve into your heart has narrowed and does not work properly. Traditionally, open heart surgery has been the main treatment option for aortic stenosis. However TAVI/TAVR is a newer, far less invasive alternative.
Your doctor has recommended you undergo a procedure called a transcatheter aortic valve implant/replacement (TAVI/TAVR).
You might not have heard this medical term before now and may be feeling unsure about the nature of the procedure.
This information sheet will outline what the procedure involves and what preparations and risks are involved.
After you read this information sheet, you might still have questions. If you do, please contact the team at Heart HQ. We’re here to help.
What’s a TAVI/TAVR?
If you have been diagnosed with a condition called aortic stenosis, the aortic valve into your heart has narrowed and does not work properly. The aortic valve is very important as it is a one-way valve that allows blood to flow from your heart to the rest of your body.
The aortic valve is usually a flexible structure but can narrow, leak or harden over time. These changes can be due to age, genetic factors, high blood pressure, calcium build up, cholesterol, smoking, infections or may be present at birth.
You may have experienced symptoms such as shortness of breath, chest discomfort, fatigue and dizziness which are all associated with aortic valve disease.
Traditionally, open heart surgery has been the main treatment option for aortic stenosis. However, TAVI/TAVR is a newer, far less invasive alternative.
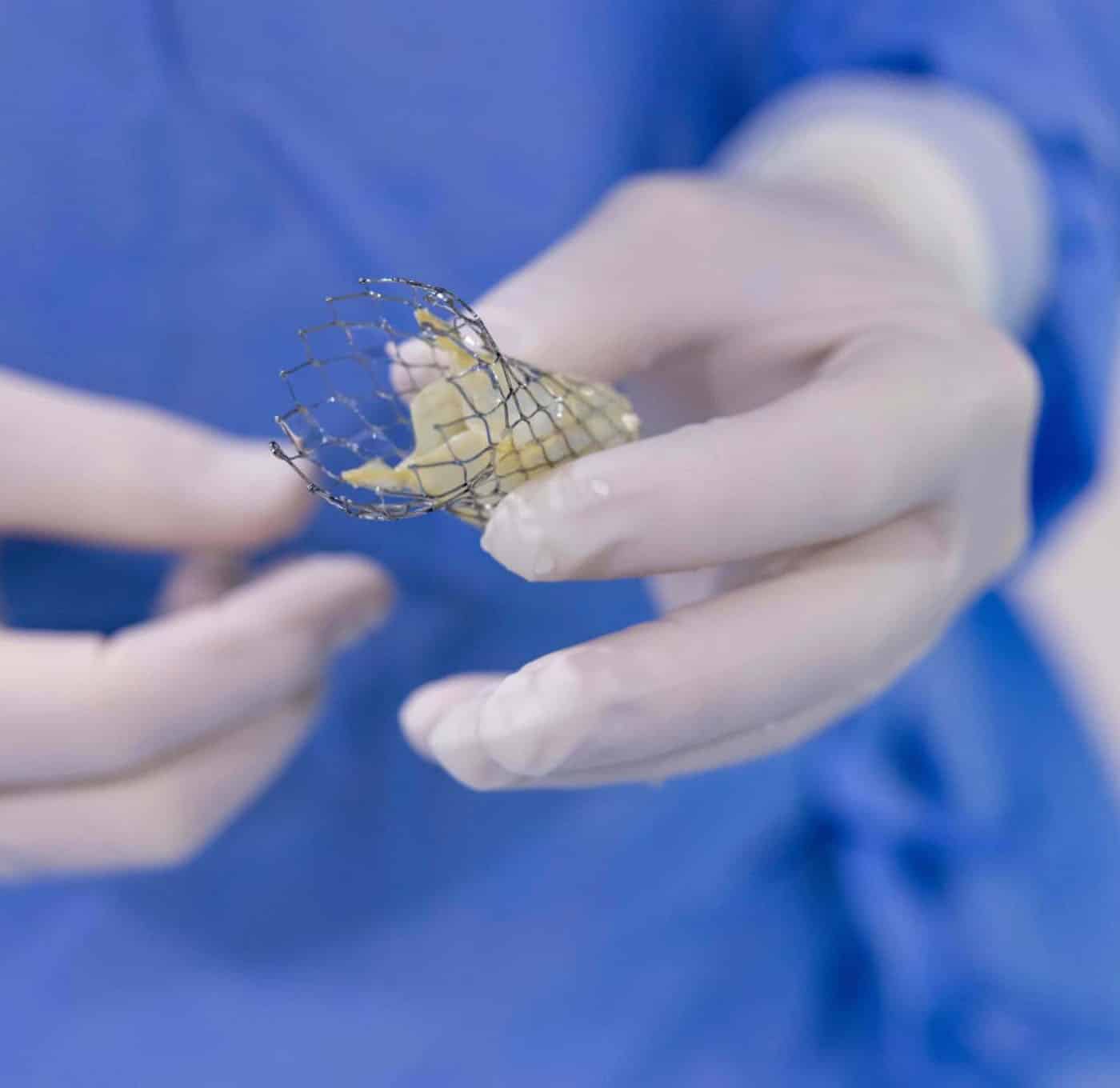
TAVI is a way of replacing your existing valve with an artificial tissue valve. A successful procedure will relieve you of symptoms of aortic stenosis, improving the quality of your life and potentially increase your life expectancy.
There are two types of valve implants and your doctor will discuss the appropriate choice for you.
How does it work?
TAVI is performed by our expert heart valve team at Sunshine Coast University Private Hospital (SCUPH). Doctors Larsen and Butterly are both accredited TAVI operators with CSANZ.
The procedure is generally performed under a special general anaesthetic provided by our expert cardiac anaesthetist. Sometimes, local anaesthetic and conscious sedation is used instead of a general anaesthetic.
An intravenous line (IV) will be placed into a vein in your arm. This is for the medical team to administer medication throughout your procedure.
Depending on the implant your cardiologist is using, you may also have a temporary pacing wire inserted into a vein in your neck or leg and passed through to the right ventricle of your heart. The pacing wire will then be externally connected to a temporary pacemaker. This will help your doctor control your heart rate during the deployment of the TAVI device. Normally the pacing wire will be removed during the procedure but on occasion it may be left in for a few days.
The TAVI device will sit inside a small metal cage known as a stent, attached to the end of the catheter. Your doctor will carefully pass the catheter via the femoral artery (the main artery at the top of your leg) up to your heart. Sometimes alternative access may be used such as the right subclavian artery in your neck/shoulder.
We perform x-rays and a transesophageal echo (an ultrasound probe inserted into your oesophagus to visualise your heart and valve during the procedure) to help visualise the positioning of the catheter and device.
Once your cardiologist is happy with the location of the TAVI, the new valve will slowly be released and will “self expand”. Alternatively, a small balloon may be used to open up the new valve.
Your diseased aortic valve will not be cut or removed in this procedure. Once completed, the catheter will be removed and the small incision site will be closed. In most cases the TAVI procedure will take about one hour but it can last up to three hours.
What happens after the procedure?
You will have further monitoring in recovery or CCU and the usual hospital stay is between one and three days.
After your procedure you’ll be required to take ongoing medication and have follow-up appointments with your doctor.
If you have any future invasive procedures, including dental treatment, make sure you let your treating doctor or dentist know about your valve replacement. You may require antibiotics before any other procedures to reduce the risk of your new valve becoming infected.
Anaesthetic
If the procedure is performed under a general anaesthetic, please arrange to have a support person (a relative or friend) collect you from hospital. You’ll also need someone to stay with you that night. You should not drive or make any important decisions in the 24 hours following general anaesthetic.
If you have any concerns about your anaesthetic, please discuss them with your doctor as soon as you can.
What kind of risks are associated with this procedure?
Any kind of procedure carries some element of risk, often very small and rare.
Your doctor has balanced the benefits and risks of carrying out the test against the benefits and risks of not proceeding. If your doctor has recommended this procedure, they believe there is benefit to you going ahead.
It’s important you understand the risks involved so you can make an informed decision.
Here are the most commonly reported risks and complications associated with a TAVI/TAVR procedure.
Common risks and complications (more than 5% of cases)
- Swelling, bruising or haematoma at the puncture site
- Femoral artery aneurysm or pseudoaneurysm (false aneurysm)—this may require surgical repair or stent placement
- Hypertension or hypotension (high or low blood pressure)
- Abnormal heart rhythms—a permanent pacemaker may be required
- Bleeding from the groin—a blood transfusion may be required
- Increased risk of wound infection, chest infection, heart and lung complications, and blood clot in the leg or lungs for people who are obese
Uncommon risks and complications (1–5% of cases)
- Infection requiring antibiotics
- Worsening or failure of kidney function sometimes requiring dialysis
- Stroke (blood clot or bleeding in the brain) which may cause permanent disability
- Heart attack caused by the new valve blocking the coronary arteries
- Lung collapse—this may need antibiotics, physiotherapy or tube insertion to remove air or fluid from the chest
- Blood clot in the leg causing pain and swelling—in rare cases part of the clot may dislodge and go to the lungs
Rare risks and complications (less than 1% of cases)
- Perforation or damage of vessels, myocardium (heart muscle) or valve structures which may require emergency major surgery
- Valve moving from where it was initially placed—the valve may need to be removed with a special catheter or open heart surgery
- Opening or tear in the lining of the aorta (aortic dissection)
- Infection settling on the new valve (endocarditis)
- Significant leakage around the new valve
- Death as a result of this procedure is rare
There may also be risks specific to your individual condition and circumstances. Please talk with your doctor about any concerns you might have.
Transcatheter aortic valve implant/replacement info sheet